Pericardial Effusion: Diagnosis And Treatment
The accumulation of fluid in the pericardium is the state in which fluid accumulates around the heart. Sometimes it is related to a disease, but sometimes more detailed research is needed to find out the cause. In some cases, the cause is not determined. In fact, it can even become chronic without causing serious problems. Getting treatment is still very important.
Typically, treatment focuses on treating the cause of the pericardial effusion and controlling the symptoms. But if its cause is unknown, the treatment is the same as for pericarditis, or inflammation of the pericardium.
What is the fluid accumulation in the pericardium?

Cardiac sac fluid accumulation means abnormal accumulation of fluid in the pericardial cavity. The pericardium consists of two leaves: a layer of serous and connective tissue. Between the two leaves is a pericardial cavity where tissue fluid is normally no more than 50 ml. During the inflammatory process, fluid production increases and fluid accumulation in the pericardium develops.
This can also occur as fluid reabsorption decreases. This is generally due to elevated systemic venous pressure. This increase in pressure is typically due to heart failure or elevated pulmonary blood pressure.
Diagnosis
The symptoms of fluid accumulation in the pericardium depend on how quickly fluid accumulates. Typical symptoms include shortness of breath and chest pain. Other common symptoms include nausea, difficulty swallowing, hoarseness, and hiccups.
When your doctor suspects that you have accumulated fluid in your pericardium, you may need one or more of the following tests:
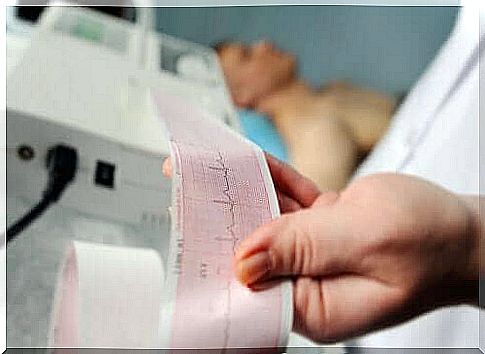
- Cardiac ultrasound. This allows the doctor to determine the extent of fluid retention and assess heart function.
- Electrocardiogram. This test can detect possible blockages.
- Chest X-ray. With this method, the doctor can find out how extensive the fluid accumulation in the pericardium is.
The most commonly used diagnostic method is ultrasound. However, a broader picture of the situation can be obtained by computed tomography or magnetic resonance imaging. However, due to availability and cost, these are not used so often.
In any case, cardiac imaging helps to determine five key factors: size, duration, prevalence, composition, and hemodynamic effects. These are used to determine the cause of pericardial effusion to determine appropriate treatment.
Pericardial effusion: treatment

The treatment of pericardial fluid accumulation generally depends on several different factors: the amount of fluid accumulated, the possible tamponing of the heart, and the cause of the problem. In general, the problem disappears as soon as the cause is treated.
The first step in treating pericardial fluid accumulation is to assess its size. Your doctor should also assess its effect on your bloodstream and find out any possible comorbidities. An estimated 60% of cases have an underlying cause of pericardial effusion. If there is no tamponing or a high risk of it occurring, most doctors will prescribe bed rest and NSAIDs. Colchicine and corticosteroids are also often prescribed.
If there is a risk of tamponing or a high risk of worsening fluid retention, a pericardial stenosis is performed. When this cannot be done or fails, the next step is to drain the fluid with open surgery. To do this, take a test piece and make an opening in the heart bag.
Status monitoring and forecast
Idiopathic pericardial effusion and pericarditis have a good prognosis. The risk of complications is therefore very low. In chronic idiopathic pericardial effusion, the probability of cardiac tamponade is 30-35%. In the second type of fluid accumulation, the prognosis depends mainly on its cause and size. In approximately one-third of all cases, those greater than 10 mm worsen and develop into tampons.
It is recommended to monitor moderate idiopathic fluid accumulation with cardiac ultrasound every six months. In severe cases, imaging should be done every three months. In non-idiopathic cases, monitoring of the patient’s condition depends on the cause of the disease.